DVT (Deep Vein Thrombosis)
- Created in Ball/Joint/Tendon
 Deep Vein Thrombosis (DVT) is a serious medical condition that occurs when a blood clot forms in a deep vein, typically in the lower limbs. This condition poses significant health risks, including the potential for the clot to dislodge and travel to the lungs, causing a life-threatening condition known as pulmonary embolism. In this comprehensive guide, we will explore the intricacies of DVT, shedding light on its causes, symptoms, diagnostic approaches, and effective prevention strategies. By providing a deeper understanding of this condition, we aim to empower readers with the knowledge to recognize, address, and reduce the risk of DVT.
Deep Vein Thrombosis (DVT) is a serious medical condition that occurs when a blood clot forms in a deep vein, typically in the lower limbs. This condition poses significant health risks, including the potential for the clot to dislodge and travel to the lungs, causing a life-threatening condition known as pulmonary embolism. In this comprehensive guide, we will explore the intricacies of DVT, shedding light on its causes, symptoms, diagnostic approaches, and effective prevention strategies. By providing a deeper understanding of this condition, we aim to empower readers with the knowledge to recognize, address, and reduce the risk of DVT.
Defining Deep Vein Thrombosis (DVT)
What is DVT?
Deep Vein Thrombosis is a medical condition characterized by the formation of blood clots in deep veins, usually within the legs. These clots can impede blood flow, causing various complications and posing a risk of serious health consequences.
How Does DVT Occur?
DVT often develops when blood flow is slow or sluggish, allowing blood cells to clump together and form a clot. Several factors contribute to this condition, ranging from immobility and surgery to underlying medical conditions that affect blood clotting.
Causes and Risk Factors
Prolonged Immobility
Extended periods of immobility, such as during long flights, bed rest, or extended hospital stays, increase the risk of DVT. Reduced movement hinders blood circulation, fostering conditions conducive to clot formation.
Surgery and Trauma
Certain surgeries, particularly those involving the lower limbs or abdomen, can elevate the risk of DVT. Trauma or injury that damages blood vessels may also contribute to clot formation.
Medical Conditions and Genetics
Medical conditions such as cancer, inflammatory disorders, and genetic factors that affect blood clotting can predispose individuals to DVT. Understanding these underlying factors is crucial for effective prevention and management.
Recognizing Symptoms of DVT
Swelling and Pain
One of the primary symptoms of DVT is swelling, often accompanied by pain or tenderness in the affected leg. The swelling may be sudden and is typically localized to one leg.
Warmth and Discoloration
The skin over the affected area may feel warm to the touch, and the skin color may change, appearing reddish or bluish. These signs indicate compromised blood flow in the affected vein.
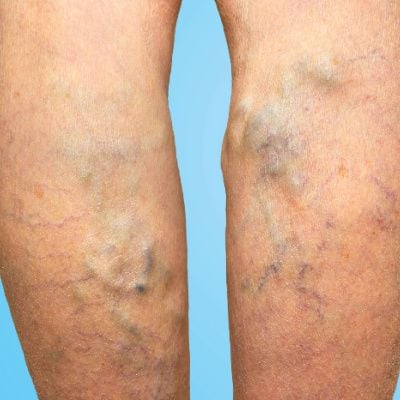
Enlarged Veins
In some cases, the superficial veins near the surface of the skin may become more visible or enlarged. This is known as superficial thrombophlebitis and can be associated with DVT.
Diagnosing DVT
Ultrasound Imaging
Ultrasound imaging is the most common and effective method for diagnosing DVT. It allows healthcare professionals to visualize blood flow and detect the presence of clots in the deep veins.
D-Dimer Test
The D-Dimer blood test measures the presence of a substance released when a blood clot breaks up. Elevated D-Dimer levels may indicate the presence of an active blood clot, prompting further investigation.
Venography and MRI
In certain cases, venography or magnetic resonance imaging (MRI) may be employed to provide detailed images of the veins and identify the location and extent of the clot.
Treatment Approaches for DVT
Anticoagulant Medications
The primary treatment for DVT involves anticoagulant medications, commonly known as blood thinners. These medications prevent the clot from growing larger and reduce the risk of additional clots forming.
Compression Stockings
Wearing compression stockings helps alleviate swelling and promotes blood circulation in the legs. These stockings provide external pressure to prevent blood from pooling and clot formation.
Thrombolytic Therapy
In severe cases, where a large clot poses an immediate threat, thrombolytic therapy may be considered. This involves medications that dissolve the clot, restoring normal blood flow.
Preventing DVT
Physical Activity
Regular physical activity, especially during long periods of sitting or immobility, is crucial for preventing DVT. Simple leg exercises and regular breaks during travel or sedentary activities can make a significant difference.
Compression Garments
For individuals at higher risk of DVT, such as those with a history of the condition or undergoing surgery, wearing compression garments may be recommended to support healthy blood flow.
Hydration
Staying adequately hydrated is essential for maintaining optimal blood viscosity. Dehydration can contribute to sluggish blood flow, increasing the risk of clot formation.
Living with DVT
Lifestyle Modifications
Individuals with a history of DVT may need to make lifestyle modifications, including maintaining a healthy weight, avoiding tobacco use, and managing underlying medical conditions that contribute to clotting.
Regular Follow-Up
Regular follow-up appointments with healthcare providers are crucial for monitoring blood clotting parameters, adjusting medications as needed, and addressing any emerging concerns or symptoms.
Emotional and Psychological Impact
Coping Strategies
A diagnosis of DVT can have emotional and psychological implications. Implementing coping strategies, seeking support from healthcare professionals, and connecting with support groups contribute to overall well-being.
Education and Awareness
Raising awareness about DVT within communities helps combat misconceptions and promotes proactive measures for prevention. Education about risk factors and symptoms empowers individuals to take charge of their vascular health.
Seeking Professional Guidance
Vascular Specialists
Consulting with vascular specialists or healthcare professionals with expertise in clotting disorders ensures a comprehensive assessment and personalized treatment plan. Regular follow-ups are essential for ongoing management.
Patient Advocacy Groups
Engaging with patient advocacy groups provides valuable resources, support, and a sense of community for individuals living with or at risk of DVT.
Conclusion
In conclusion, Deep Vein Thrombosis is a serious vascular condition that requires prompt recognition, intervention, and ongoing management. By understanding the causes, recognizing symptoms, and adopting preventive measures, individuals can significantly reduce the risk of DVT and its associated complications. Through a combination of lifestyle modifications, medical interventions, and ongoing healthcare support, individuals can lead fulfilling lives while effectively managing the challenges posed by DVT. Proactive measures, coupled with awareness and education, form the cornerstone of a comprehensive approach to vascular health.
Disclaimer:
The information on this website is provided for educational and information purposes only and is not medical advice. Always consult with a licensed medical provider and follow their recommendations regardless of what you read on this website. If you think you are having a medical emergency, dial 911 or go to the nearest emergency room. Links to other third-party websites are provided for your convenience only. If you decide to access any of the third-party websites, you do so entirely at your own risk and subject to the terms of use for those websites. Neither Sheldon H. Nadal, D.P.M., nor any contributor to this website, makes any representation, express or implied, regarding the information provided on this website or any information you may access on a third-party website using a link. Use of this website does not establish a doctor-patient relationship. If you would like to request an appointment with a health care provider, please call our office at (416) 486-9917.

